How To Set Up A Blood Drive At Work
Do y'all e'er wonder what makes up blood? Unless y'all need to take blood drawn, donate it or have to stop its flow afterward an injury, you probably don't think much about it. Simply blood is the most usually tested part of the body, and information technology is truly the river of life. Every jail cell in the trunk gets its nutrients from blood. Understanding blood will help y'all as your medico explains the results of your claret tests. In addition, you lot will learn amazing things about this incredible fluid and the cells in it.
Claret is a mixture of ii components: cells and plasma. The centre pumps blood through the arteries, capillaries and veins to provide oxygen and nutrients to every prison cell of the trunk. The claret besides carries abroad waste products.
The developed man trunk contains approximately 5 liters (v.iii quarts) of blood; it makes up seven to 8 percent of a person's body weight. Approximately 2.75 to 3 liters of blood is plasma and the remainder is the cellular portion.
Plasma is the liquid portion of the claret. Blood cells like red blood cells float in the plasma. As well dissolved in plasma are electrolytes, nutrients and vitamins (captivated from the intestines or produced by the body), hormones, clotting factors, and proteins such as albumin and immunoglobulins (antibodies to fight infection). Plasma distributes the substances it contains equally it circulates throughout the torso.
The cellular portion of blood contains ruby blood cells (RBCs), white blood cells (WBCs) and platelets. The RBCs deport oxygen from the lungs; the WBCs help to fight infection; and platelets are parts of cells that the body uses for clotting. All claret cells are produced in the bone marrow. Equally children, most of our bones produce blood. Equally we age this gradually diminishes to just the basic of the spine (vertebrae), breastbone (sternum), ribs, pelvis and small-scale parts of the upper arm and leg. Bone marrow that actively produces blood cells is called red marrow, and bone marrow that no longer produces blood cells is called yellow marrow. The process past which the body produces claret is called hematopoiesis. All blood cells (RBCs, WBCs and platelets) come from the same type of cell, called the pluripotential hematopoietic stem prison cell. This grouping of cells has the potential to grade whatever of the dissimilar types of blood cells and as well to reproduce itself. This jail cell then forms committed stalk cells that will form specific types of blood cells.
Nosotros'll learn more about red blood cells in detail next.
Cerise Blood Cells

Photo courtesy Garrigan.Net
Microscopic image of red claret cells
During formation, the RBC eventually loses its nucleus and leaves the bone marrow as a reticulocyte. At this point, the reticulocyte contains some remnants of organelles. Somewhen these organelles go out the cell and a mature erythrocyte is formed. RBCs terminal an boilerplate of 120 days in the bloodstream. When RBCs historic period, they are removed past macrophages in the liver and spleen.
A hormone called erythropoietin and low oxygen levels regulate the production of RBCs. Any factor that decreases the oxygen level in the body, such as lung disease or anemia (depression number of RBCs), increases the level of erythropoietin in the torso. Erythropoietin then stimulates production of RBCs past stimulating the stem cells to produce more than RBCs and increasing how quickly they mature. Ninety per centum of erythropoietin is made in the kidneys. When both kidneys are removed, or when kidney failure is present, that person becomes anemic due to lack of erythropoietin. Iron, vitamin B-12 and folate are essential in the product of RBCs.
Blood-red blood cells (RBCs) are by far the about abundant cells in the blood. RBCs give blood its characteristic red color. In men, there are an boilerplate of 5,200,000 RBCs per cubic millimeter (microliter), and in women there are an boilerplate of 4,600,000 RBCs per cubic millimeter. RBCs business relationship for approximately forty to 45 percentage of the blood. This percentage of blood fabricated up of RBCs is a often measured number and is called the hematocrit. The ratio of cells in normal claret is 600 RBCs for each white blood cell and xl platelets.
There are several things about RBCs that make them unusual:
- An RBC has a strange shape -- a biconcave disc that is circular and flat, sort of like a shallow basin.
- An RBC has no nucleus. The nucleus is extruded from the jail cell every bit it matures.
- An RBC can change shape to an amazing extent, without breaking, as it squeezes single file through the capillaries. (Capillaries are infinitesimal blood vessels through which oxygen, nutrients and waste products are exchanged throughout the trunk.)
- An RBC contains hemoglobin, a molecule particularly designed to hold oxygen and carry it to cells that need it.
The primary part of red claret cells is to transport oxygen from the lungs to the cells of the body. RBCs comprise a protein chosen hemoglobin that actually carries the oxygen.
In the capillaries, the oxygen is released to be used by the cells of the body. Xc-seven per centum of the oxygen that is carried past the blood from the lungs is carried by hemoglobin; the other three percent is dissolved in the plasma. Hemoglobin allows the blood to send 30 to 100 times more oxygen than could exist dissolved in the plasma lonely.
Hemoglobin combines loosely with oxygen in the lungs, where the oxygen level is high, and so hands releases it in the capillaries, where the oxygen level is depression. Each molecule of hemoglobin contains four fe atoms, and each iron atom can bind with one molecule of oxygen (which contains two oxygen atoms, chosen O2) for a total of four oxygen molecules (4 * O2) or 8 atoms of oxygen for each molecule of hemoglobin. The iron in hemoglobin gives blood its carmine color.
Xxx-three percent of an RBC is hemoglobin. The normal concentration of hemoglobin in claret is 15.5 grams per deciliter of claret in men, and 14 grams per deciliter of blood in women. (A deciliter is 100 milliliters, or one-tenth of a liter.)
Besides carrying oxygen to the cells of the trunk, the RBCs help to remove carbon dioxide (CO2) from the torso. Carbon dioxide is formed in the cells as a byproduct of many chemical reactions. Information technology enters the claret in the capillaries and is brought dorsum to the lungs and released there and then exhaled as we breathe. RBCs contain an enzyme called carbonic anhydrase which helps the reaction of carbon dioxide (CO2) and water (HtwoO) to occur 5,000 times faster. Carbonic acid is formed, which then separates into hydrogen ions and bicarbonate ions:
COii + H2O ===> H2CO3 + H+ + HCOiii -
carbon dioxide + water ==> carbonic acid + hydrogen ion + bicarbonate ion
The hydrogen ions then combine with hemoglobin and the bicarbonate ions go into the plasma. Seventy pct of the CO2 is removed in this way. Vii percent of the COii is dissolved in the plasma. The remaining 23 pct of the COii combines direct with hemoglobin so is released into the lungs.
In the next section, nosotros'll larn near the dissimilar types of white claret cells.
White Claret Cells
White claret cells (WBCs), or leukocytes, are a part of the immune system and help our bodies fight infection. They circulate in the blood so that they can be transported to an area where an infection has developed. In a normal developed body there are 4,000 to 10,000 (average 7,000) WBCs per microliter of blood. When the number of WBCs in your blood increases, this is a sign of an infection somewhere in your trunk.
Here are the six principal types of WBCs and the boilerplate percent of each type in the blood:
- Neutrophils - 58 percent
- Eosinophils - 2 percentage
- Basophils - 1 percent
- Bands - 3 percent
- Monocytes - 4 pct
- Lymphocytes - 4 percent
Nearly WBCs (neutrophils, eosinophils, basophils and monocytes) are formed in the os marrow. Neutrophils, eosinophils and basophils are likewise called granulocytes because they have granules in their cells that incorporate digestive enzymes. Basophils take imperial granules, eosinophils have orangish-red granules and neutrophils have a faint blueish-pink colour. When a granulocyte is released into the blood, it stays there for an average of four to viii hours and then goes into the tissues of the body, where it lasts for an average of 4 to v days. During a astringent infection, these times are often shorter.
Neutrophils are the 1 of the torso's master defenses against bacteria. They kill bacteria past actually ingesting them (this is called phagocytosis). Neutrophils can phagocytize five to 20 bacteria in their lifetime. Neutrophils have a multi-lobed, segmented or polymorphonuclear nucleus and and so are also called PMNs, polys or segs. Bands are immature neutrophils that are seen in the blood. When a bacterial infection is present, an increase of neutrophils and bands are seen.
Eosinophils kill parasites and have a role in allergic reactions.
Basophils are non well understood, merely they office in allergic reactions. They release histamine (which causes claret vessels to leak and attracts WBCs) and heparin (which prevents clotting in the infected surface area so that the WBCs tin reach the bacteria).
Monocytes enter the tissue, where they get larger and turn into macrophages. There they can phagocytize leaner (upwardly to 100 in their lifetime) throughout the body. These cells also destroy old, damaged and dead cells in the body. Macrophages are found in the liver, spleen, lungs, lymph nodes, skin and intestine. The system of macrophages scattered throughout the body is called the reticuloendothelial system. Monocytes stay in the blood for an average of 10 to twenty hours and then get into the tissues, where they become tissue macrophages and tin alive for months to years.
Neutrophils and monocytes apply several mechanisms to get to and kill invading organisms. They can squeeze through openings in blood vessels by a process chosen diapedesis. They move effectually using ameboid motility. They are attracted to certain chemicals produced past the allowed organization or by leaner and migrate toward areas of higher concentrations of these chemicals. This is called chemotaxis. They kill leaner past a process called phagocytosis, in which they completely surround the bacteria and digest them with digestive enzymes.
In the side by side section, we'll take a closer look at lymphocytes and platelets.
Lymphocytes and Platelets
Lymphocytes are complex cells that direct the body's immune arrangement. T lymphocytes showtime in the bone marrow from pluripotent hematopoietic stem cells, then travel to and mature in the thymus gland. The thymus is located in the chest between the center and sternum (breastbone). B lymphocytes mature in the bone marrow.
T lymphocytes (T cells) are responsible for cell-mediated immunity. B lymphocytes are responsible for humoral immunity (antibody product). Seventy-five percent of lymphocytes are T cells. Lymphocytes are different from the other WBCs because they can recognize and accept a retentiveness of invading leaner and viruses. Lymphocytes continually pass back and forth between lymph tissue, lymph fluid and blood. When they are nowadays in the claret, they stay for several hours. Lymphocytes can live for weeks, months or years.
In that location are many types of T cells that have specific functions, including:
- Helper T cells - Helper T cells have proteins on their cell membranes called CD4. Helper T cells direct the rest of the immune system by releasing cytokines. Cytokines stimulate B cells to grade plasma cells, which form antibodies, stimulate the production of cytotoxic T cells and suppressor T cells and activate macrophages. Helper T cells are the cells the AIDS virus attacks -- y'all can imagine that destroying the cells that direct the immune organisation has a devastating effect.
- Cytotoxic T cells - Cytotoxic T cells release chemicals that interruption open up and impale invading organisms.
- Memory T cells - Memory T cells remain subsequently to aid the immune organization respond more rapidly if the same organism is encountered again.
- Suppressor T cells - Suppressor T cells suppress the immune response so that it does not exit of control and destroy normal cells in one case the allowed response is no longer needed.
B cells become plasma cells when exposed to an invading organism or when activated by helper T cells. B cells produce large numbers of antibodies (also chosen immunoglobulins or gamma globulins). There are 5 types of immunogloulins (abbreviated Ig): IgG, IgM, IgE, IgA and IgD. These are Y-shaped molecules that take a variable segment that is a binding site for merely one specific antigen. These bind to antigens, which causes them to clump, be neutralized or break open. They as well activate the complement organisation.
The complement system is a series of enzymes that assistance or complement antibodies and other components of the immune organisation to destroy the invading antigen by alluring and activating neutrophils and macrophages, neutralizing viruses and causing invading organisms to break open. Retentivity B cells likewise remain for prolonged periods, and if the aforementioned antigen is encountered it causes a more rapid response in producing antibodies.
Platelets (thrombocytes) assistance claret to clot by forming something called a platelet plug. The other fashion that blood clots is through coagulation factors. Platelets likewise help to promote other blood clotting mechanisms. There are approximately 150,000 to 400,000 platelets in each microliter of blood (average is 250,000).
Platelets are formed in the bone marrow from very large cells called megakaryocytes, which suspension upwardly into fragments -- these cellular fragments are platelets. They do not have a nucleus and practise not reproduce. Instead, megakaryocytes produce more platelets when necessary. Platelets generally last for an average of 10 days.
Platelets contain many chemicals that assist clotting. These include:
- Actin and myosin, to assistance them contract
- Chemicals that help the coagulation process to begin
- Chemicals that attract other platelets
- Chemicals that stimulate blood vessel repair
- Chemicals that stabilize a blood jell
Plasma
Plasma is a clear, yellowish fluid (the color of straw). Plasma can sometimes appear milky afterwards a very fatty meal or when people have a high level of lipids in their blood. Plasma is 90-percent h2o. The other 10 percent dissolved in plasma is essential for life. These dissolved substances are circulated throughout the torso and lengthened into tissues and cells where they are needed. They diffuse from areas of loftier concentration to areas of lower concentration. The greater the difference in concentration, the greater the amount of material that diffuses. Waste materials flow in the contrary management, from where they are created in the cells into the bloodstream, where they are removed either in the kidneys or lungs.
Hydrostatic pressure (blood pressure) pushes fluid out of blood vessels. Balancing this is something called oncotic force per unit area (caused by proteins dissolved in blood), which tends to go along fluid inside the blood vessels.
Proteins make up a large part of the 10 percent of material dissolved in plasma and are responsible for oncotic pressure. Protein molecules are much larger than water molecules and tend to stay in blood vessels. They have more difficulty fitting through the pores in capillaries, and therefore have a higher concentration in blood vessels. Proteins tend to attract water to go on their relative concentration in blood vessels more in line with fluid outside the blood vessels. This is one of the means the body maintains a constant book of claret.
Plasma contains 6.v to viii.0 grams of poly peptide per deciliter of blood. The principal proteins in plasma are albumin (sixty percent), globulins (alpha-1, alpha-2, beta, and gamma globulins (immunoglobulins)), and clotting proteins (especially fibrinogen). These proteins function to maintain oncotic pressure (especially albumin) and ship substances such as lipids, hormones, medications, vitamins, and other nutrients. These proteins are also part of the immune system (immunoglobulins), assistance blood to clot (clotting factors), maintain pH residual, and are enzymes involved in chemical reactions throughout the body.
Electrolytes are another large category of substances dissolved in plasma. They include:
- Sodium (Na+)
- Potassium (K+)
- Chloride (Cl-)
- Bicarbonate (HCO3 -)
- Calcium (Ca+2)
- Magnesium (Mg+2)
These chemicals are absolutely essential in many bodily functions including fluid residuum, nerve conduction, muscle contraction (including the eye), blood clotting and pH remainder.
Other materials dissolved in plasma are carbohydrates (glucose), cholesterol, hormones and vitamins. Cholesterol is ordinarily transported attached to lipoproteins such as low-density lipoproteins (LDLs) and loftier-density lipoproteins (HDLs). For more information on cholesterol, read How Cholesterol Works.
When plasma is allowed to clot, the fluid left behind is called serum. When claret is collected from a patient it is immune to jell in a test tube, where the cells and clotting factors autumn to the bottom and the serum is left on elevation. Serum is tested for all the numerous items discussed above to determine if any abnormalities exist.
Claret Types
There are four major claret types: A, B, AB, and 0. The claret types are determined by proteins called antigens (also called agglutinogens) on the surface of the RBC.
U.S. Blood Blazon Distribution
According to the American Association of Blood Banking, these are the percentages of different claret types in the U.S. population:
- A+: 34 per centum
- A-: 6 percent
- B+: 9 percent
- B-: ii percent
- AB+: 3 percent
- AB-: ane percent
- O+: 38 percent
- O-: 7 pct
There are two antigens, A and B. If you have the A antigen on the RBC, then you have type A blood. When B antigen is present, yous have type B blood. When both A and B antigens are nowadays, you take blazon AB blood. When neither are nowadays, yous have type O claret.
When an antigen is present on the RBC, and so the opposite antibody (too called agglutinin) is present in the plasma. For case, type A blood has anti-blazon-B antibodies. Type B blood has anti-type-A antibodies. Type AB blood has no antibodies in the plasma, and type O blood has both anti-type-A and anti-type-B antibodies in the plasma. These antibodies are non nowadays at birth only are formed spontaneously during infancy and last throughout life.
In addition to the ABO blood grouping system, in that location is an Rh blood group system. In that location are many Rh antigens that can be present on the surface of the RBC. The D antigen is the nearly common Rh antigen. If the D antigen is present, then that claret is Rh+. If the D antigen is missing, then the blood is Rh-. In the United States, 85 percent of the population is Rh+ and 15 percent is Rh-. Unlike in the ABO arrangement, the corresponding antibody to the Rh antigen does not develop spontaneously but simply when the Rh- person is exposed to Rh antigen by blood transfusion or during pregnancy. When an Rh- female parent is meaning with an Rh+ fetus, and so the mother forms antibodies that can travel through the placenta and cause a illness called hemolytic affliction of the newborn (HDN), or erythroblastosis fetalis.
Donating Blood
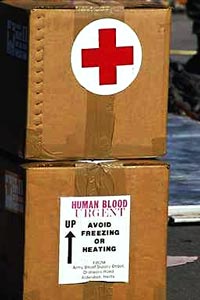
Ruddy Cantankerous blood supplies sent to the Gulf during the Gulf War
A unit of blood is 1 pint (450 milliliters) and is mixed with chemicals (CPD) to prevent clotting. Each yr, approximately 12 million to 14 meg units of blood are donated in the United States. Generally, a claret donor must be at to the lowest degree 17 years old, exist healthy, and weigh over 110 pounds.
Prior to donating blood, the donor is given an information pamphlet to read. A health history is taken to ensure that the donor has not been exposed to diseases that can be transmitted by claret, and to decide if altruistic blood is safe for that person's own health. The donor's temperature, pulse, claret pressure and weight are obtained. A few drops of blood are obtained to brand sure the donor is not anemic. Information technology usually takes less than 10 minutes for the claret to exist removed once the needle has been placed. Sterile, single-use equipment is used so there is no danger of infection to the donor. Donors should drink extra fluids and avoid exercise that day. Blood can be donated every 8 weeks.
Autologous claret donation is the donation of claret for 1's own utilize, commonly prior to surgery. Apheresis is the procedure in which only a specific component of a donor'south blood is removed (normally platelets, plasma or leukocytes). In this way, more of that specific component can be removed than can be derived from one unit of claret.
Each unit of blood can exist separated into several components so that each component tin be given to someone with a need for that specific 1. Therefore, a single unit of blood can help many people. These components include:
- Packed RBCs
- Fresh frozen plasma
- Platelets
- WBCs
- Albumin
- Immunoglobulins
- Cryoprecipitate anti-hemolytic factor
- Factor 8 concentrate
- Factor Ix concentrate
Permit's look at each of these blood components in more than detail.
Red blood cells (packed RBCs)
Plasma (fresh frozen plasma), once thawed, is transfused to treat bleeding disorders when many clotting factors are missing. This occurs in liver failure, when too much of a claret thinner called Coumadin has been given, or when severe haemorrhage and massive transfusions upshot in low levels of clotting factors.
Platelets are transfused in people with depression platelet count (thrombocytopenia) or abnormally functioning platelets. Each unit of platelets raises the platelet count by approximately 5,000 platelets per microliter of blood.
Albumin makes up 60 pct of the poly peptide in plasma, is produced in the liver and is used when blood volume needs to be increased and fluids have non worked, equally in cases of astringent bleeding, liver failure and severe burns.
Immunoglobulins are given to persons who have been exposed to a sure illness such as rabies, tetanus or hepatitis to assist prevent that disease.
Factor VIII concentrate and cryoprecipitate are used in hemophilia A (classic hemophilia) since this is acquired by a factor VIII deficiency.
Factor Ix concentrate is used in hemophilia B ("Christmas disease"), which is caused by a deficiency of clotting factor Ix.
Ensuring a Prophylactic Claret Supply
There are many tests that are performed on blood to ensure its safe. These tests include checking for:
- Hepatitis B surface antigen
- Hepatitis B core antibody
- Hepatitis C antibody
- HIV-1, HIV-2 antibodies
- HIV-1 p24 antigen
- HTLV-one, HTLV-2 antibodies
- Syphilis
If any of these tests are positive, the blood is discarded. As of 1996, the gamble of getting HIV from a unmarried blood transfusion was 1 in 676,000 units of blood, the take a chance of developing Hepatitis B was 1 in 66,000 units and the hazard of getting Hepatitis C was 1 in 100,000 units. However, newer testing may decrease the run a risk of Hepatitis C to between 1 in 500,000 and 1 in 1,000,000.
When blood is transfused into a patient, the blood type must be adamant so that a transfusion reaction does non occur.
A reaction occurs when the antigens on the RBCs of the donor blood react with the antibodies present in the recipient'due south plasma. In other words, if donor blood of blazon A (contains A antigens) is given to someone with type B blood (they take anti-type A antibodies in their claret), then a transfusion reaction will occur.
The contrary does not occur. It is unusual for the antibodies in the plasma of the donated blood to react to the antigens on the recipients RBCs because very lilliputian plasma is transfused and it gets diluted to a level too low to cause a reaction.
When a transfusion reaction occurs, an antibody attaches to antigens on several RBCs. This causes them to clump together and plug upwardly blood vessels. Then they are destroyed past the torso (called hemolysis), releasing hemoglobin from the RBCs into the claret. Hemoglobin is broken down into bilirubin, which tin cause jaundice. These events occur in hemolytic disease of the newborn (mentioned previously).
When an emergency blood transfusion is necessary and the recipient's blood type is unknown, anyone can get type O- blood transfused since type O- blood has no antigen on its surface that could react with antibodies in the recipient's plasma. Therefore, someone with type O- blood is called a universal donor. Someone with type AB claret is called a universal recipient because they take no antibodies that could react with donated blood.
For more than information on claret and related topics, bank check out the links on the next folio.
Originally Published: Apr one, 2000
How Blood Works FAQ
What is a normal platelet count?
A normal platelet count ranges from 150,000 to 450,000 platelets per microliter of claret. More than 450,000 indicates a condition called thrombocytosis while having fewer than 150,000 is known as thrombocytopenia.
What is the function of cherry claret cells?
The chief part of red blood cells is to ship oxygen from the lungs to the residual of the body. They too assistance to remove carbon dioxide (CO2) from the body, transporting information technology in the claret through the capillaries back to the lungs, releasing information technology there to be exhaled.
What are the ii components of blood?
Blood is a mixture of two components: cells and plasma. The cellular portion of blood contains ruby-red blood cells, white blood cells, and platelets while the plasma is the liquid portion. Of the five liters (5.3 quarts) of blood in an adult human body, approximately 2.75 to 3 liters of claret is plasma and the balance is cellular.
What are the claret types?
The eight nearly common blood types are A+, A-, B+, B-, O+, O-, AB+, AB-.
What is the part of platelets?
Platelets help blood to clot by forming something called a platelet plug. When they recognize damaged blood vessels in an expanse of the body, they bind together.
Lots More than Information
Source: https://health.howstuffworks.com/human-body/systems/circulatory/blood.htm

0 Response to "How To Set Up A Blood Drive At Work"
Post a Comment